Scientist Says Routine Blood Tests Might Someday Help Predict Suicide Risk
By ll
@docrioum (3)
Algiers, Algeria
August 29, 2013 5:38am CST
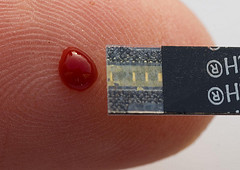
An intriguing new study on the predictability of suicide is making the rounds: A team at Indiana University School of Medicine has discovered that certain biomarkers in the blood are linked, fairly reliably, to our risk of committing suicide. Not only do they seem to point to one’s risk at present, but they may also predict the likelihood of suicide over a lifetime. So far the connection has been illustrated in people with known mental health issues, but in the future it will be tested in the general population. The study, while fascinating, begs the question of how would we actually use such tests for people with and without histories of suicidal thoughts or depression. The objectivity is alluring, but then again, how big a role should objectivity play in the realm of mental health?
The team found that there were six genes whose activity correlated strongly with high suicide ideation (suicidal thoughts) in people with bipolar disorder. That is, when the genes’ activity was high, so were suicidal thoughts. And to confirm that the connection held strong through the act of committing suicide, the researchers also looked at the blood samples of nine people who had actually committed suicide. They found evidence that the same biomarkers were increased in these individuals as well. “It works like a Google GOOG -0.19% search ranking,” Niculescu told Nature. “Those that had the most independent lines of evidence got the highest rank.” One marker, called SAT1, was “head and shoulders above the rest,” Niculescu added.
The results of the study, say some, might point to a new and more objective way of monitoring risk, since many people may not report the subjective stuff – the suicidal thoughts and ruminations – to their doctors or psychologists. It’s hard to imagine how such tests would be put into action, though, since the feasibility of regular blood work to screen for suicide seems somewhat farfetched.
But study author Alexander Niculescu envisions a couple of different scenarios for screening. He says that “for people with mental health issues, conducting regular blood tests will become routine in the future, like other areas of medicine. Then you may catch things early. For people without known mental health issues, they could be tested if there is a suspicion they may be entertaining thoughts of suicide.”
Periodically testing people with known mental health issues is one thing. Testing people without known psychological issues because a doctor suspects the one is having suicidal thoughts is stickier. How logical it would be to put any of this into action is still very much up for debate.
What might make more sense is using the tests another way. Since the markers may predict not only present risk but also long-term risk, they could conceivably call out people who are at a perpetually higher “baseline” risk. “More intriguing, and needing future exploration,” says Niculescu, “is the fact that the markers we discovered are not just state markers but seem to have a trait (long-term risk) component, as they are able to predict future hospitalizations.”
If that’s the case, he adds, doctors might one day throw in, say, a “psychiatric risk panel” along with blood fats and blood glucose, in our annual blood work. “They could be tested as part of general health routine primary care health-checks, as a screening to identify someone who might be at higher risk, just like higher levels of cholesterol can identify someone who’s at higher risk for cardiovascular disorders.”
The obvious question is what course of action a doctor would take if someone’s blood work came back with high suicide risk, but no history of depression. It’s not exactly clear, but one important point is that a blood test alone isn’t going to tell us much of anything without a number of other elements taken into account. “As in cardiovascular disorders, the context (clinical, socio-demographic, and other risk factors) matters in terms of arriving at an actionable clinical decision,” says Niculescu. So if your blood tests come back showing high suicide risk, but you don’t have any of the other risk factors, like depression or other mood disorders, major life stress, a family history, and so on, no one is going to put you on suicide watch.
How “high risk” results would even be revealed to the patient could also be a tricky topic to broach, but these are questions doctors are going to have to continue grappling with as we understand more about how risk actually works. A million people commit suicide every year, and reducing its rate has proven to be a difficult endeavor. At least we’re thinking in new and innovative ways. Whether biomarkers are going to make a dent in the problem, or whether there are more valuable ways to address it, will remain to be seen.
1 response
@cupkitties (7421)
• United States
29 Aug 13
That is actually pretty disturbing. Right up there with the thought police.